Lupus i huden: Sommerfuglutslett. Illustrasjon: By Doktorinternet – Own work, CC BY-SA 4.0
Definisjon
Forskjellige typer utslett i huden (hudsymptomer) og munnhulen forekommer hos de fleste med systemisk lupus erythematosus (SLE) og er sammen med symptomer fra ledd, muskler og sener de vanligste sykdomstegn ved SLE.
Forekomst
Hudsymptom: 20% ved debut, 50-70% senere (referanse: Sontheimer RD 1996)
Ulike typer hudaffeksjon ved lupus
Mukokutant utslett
I munnhulen forkommer slimhinneforandringer hos 25-45%. Orale ulcerasjoner (sår i munnen) hos 28%. Disse kan være svært forskjellige i størrelse, lokalisasjon og form.
- Lepper, tannkjøtt, innsiden av kinn og gane kan bli angrepet
Sommerfugl utslett (malar rash)

Sommerfugleksantem ved SLE. Uva L, Autoimmune Dis (2012). CC BY 3.0
Eksem på begge kinn og over neseryggen. Eksemet minner om formen til en sommerfugl.
- Omtrent 50% med SLE opplever et sommerfugl-utslett, vanligst etter eksponering for sol eller sterkt lys eller ved økende sykdomsaktivitet. Huden føles varm og er litt hoven
- Utslettet varer i timer eller dager og blusser ofte opp
Sykdommer som ikke er forbundet med SLE, men som gir lignende forandringer i ansiktet er:
Soleksem
Utslett på solutsatte områder. Utslettet kan ha forskjellig form og intensitet og forekommer hos ca. 60% med SLE. Blonde, blåøyde personer har lite pigment i huden og er mest utsatt. Antistoffet SSA (Ro) er disponerende faktor
- Også Roseacea (differensial diagnose) forverres av sol
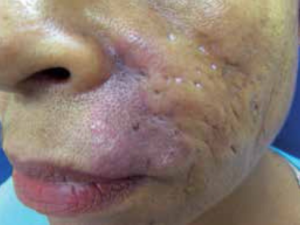
Subakutt kutan LE (SCLE)
SCLE forekommer hos omtrent 10% med SLE, men tilstanden finnes, i likhet med diskoid lupus (se nedenfor), også uten SLE
- Fotosensitivitet (soleksem)
- SSA (Ro) antistoff
- Typisk symptom-start er små rødlige, lett skjellende punkter som utvikler seg til enten psoriasis-lignende eller sirkulære former. Utslettets kanter er typisk røde, noen ganger skorpelignende. Huden over skuldre, underarmer, nakke og overkropp angripes vanligst, mens ansiktet blir spart
- SCLE er nærmere beskrevet her
Diskoid Lupus
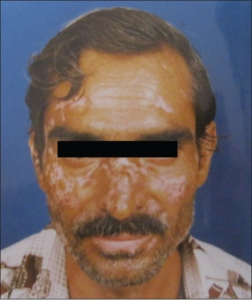
Diskoid lupus. Ranginwala AM, J Oral Maxillofac Pathol (2012) CC BY-NC-SA 3.0
Diskoid lupus blir påvist hos opptil 25% ved SLE, men forekommer også som en separat hudsykdom uten samtidig SLE. I disse tilfellene vil 5 – 10% utvikle SLE over tid
- Kjennetegn på diskoid lupus er rødlige, flassende forandringer i huden eller i hodebunnen
- Vanligst finnes forandringene i ansikt, nakke og hodebunn
- Ofte etterlates arr eller pigmentforandringer
- Diskoid lupus er ti ganger mer vanlig enn SLE
Ulike typer Diskoid Lupus
- Mucosal (slimhinner)
- Verrukøs (vorte-lignende)
- Hypertrofisk
- Teleangiektasi-lignende
Runde (Annulære) plakk (sirkulære, tørre flekker) ved Lupus kan ligne på Psoriasis
Lupus profundus / Lupsus pannikulitt

Lupus pannikulitt. Bednarek A, Postepy Dermatol Alergol (2015). CC BY-NC-ND 3.0
Pannikulitt med abscess-lignende, nekrose av fettvev under huden
- Både ansikt kropp og armer kan angripes
- Etterlater dype søkk som ligner fettatrofi etter injeksjon med kortison
- Assosiert med diskoid lupus hos 70%
- ANA påvises hos 75%
- DNA antistoff er sjelden
- Enkelte får behandling med Thalidomid
Chilblain lupus erythematosus

Chilblain lupus hos ung jente. Bansal S, Goel A – Indian Dermatol Online J (2014). CC BY-NC-SA 3.0
Blå-livide plakk/noduli på fingre
- Antistoff som ofte forekommer: ANA, SSA (Ro)
- Forekommer hos 20% med SLE
- Tilsvarende forandringer ses ved Aicardi-Goutieres syndrom (AGS)
- Behandling
- Kortison-kremer i perioder
- CellCept (mykofenolat) er rapportert å virke i enkelte tilfeller (referanse: Gouillon L, 2017)
Lupus Tumidus
Lupus tumidus. Muylaert BPB, An Bras Dermatol (2016). CC BY 4.0
Erythematøse plakk, oftest på kroppen, mindre på armer og ben
- Fotosensitivitet (soleksem) på lyseksponerte områder
- ”Intermitterende kutan lupus” (som kommer og går)
- Uspesifisert eksem:
- Urticaria/elveblest-lignende,
- Ikke kløende, kronisk urticaria 44%
- Sjelden typisk for Systemisk Lupus Erythematosus (SLE)
- Antistoff: ANA hos 30%, SSA(Ro) /SSB (La) 5%, ikke DNA
- Vevsprøve (Histologisk): Mucin-avleiring
- Assosiert med Hypo-komplement-urticaria vaskulitt (HUVS)
- Behandling med hydroksyklorokin (Plaquenil)
- Tilstanden kan være identisk eller overlappende med Jessners sykdom
STING mutasjon
- SLE-lignende forandringer i hud og vaskulitt hos barn
Lupus Pernio
Lupus Pernio er ikke relatert til Lupus, men er en form for sarkoidose i huden
Hår og hodebunn
- Hårtap (Alopesi) 20-60%, ulik grad
- Diffust hårtap vanligst, rødlig hårbunn, ikke arr, men diskoid lupus gir arr
- ”Lupus-hår”: grovt, tørt 30%. Årsaken kan være selve sykdommen, men også medikamenter og andre faktorer kan spille en rolle
Negleforandringer
Neglene kan angripes hos 25% med SLE
- Splintblødninger
- Hyperkeratose
- Dilaterte kar i negle-fold
- Pigment-forandringer
Leggsår
Kan påvises hos ca. 10% ved SLE
Vevsprøve Hudbiopsi (Stansebiopsi)
- Lyseksponert område:
- Positiv (Nedslag av immunglobulin og kompliment i dermo-epiteliale overgangssone hos 90%, men mange ”falsk positive”
- Ikke-lyseksponert:
- Mindre sensitiv, men mer spesifikk for SLE. Ved diskoid lupus forventes ikke nedslag av komplement i uaffisert hud
Forebygging og behandling av hudaffeksjon
Hensikten med behandling er å hindre varige skader i huden. Slike skader kan være mørke flekker med for mye pigment eller pigment tap, synlige blodårer (teleangiektasier), hårtap eller arr.
- Effektiv forebygging vil hindre varig skade hos de fleste
- Ømfintlige personer må beskytte huden mot sol. Beskyttelse er viktig på stranden, sjøen, innsjøer, spesielt midt på dagen (kl 10-15) når solen er sterkest.
- Solkrem med høy faktor (30 eller mer) bør brukes.
- Solbeskyttende klær kan også være aktuelt.
Medikamentell behandling er spesialistoppgave og gjøres ofte i samarbeid mellom revmatolog og hudlege. Riktig bruk av ulike medikamenter på huden er aktuelt, men også justering av den øvrige SLE behandlingen må vurderes.
- Unngå nikotin
- Solbeskyttelse
- Hydroksyklorokin (Plaquenil)
- Steroider (Prednisolon)
- Dapson brukes i sjeldne tilfeller mot bulløs SLE
- Thaliodomid i sjeldne tilfeller mot lupus profundus
- Retinoider i sjeldne tilfeller mot hypertrofisk diskoid lupus
- Behandling direkte på huden
- Steroider er førstevalg, eventuelt med okklusjon
- Takrolimus (Protopic)
- Protopic salve er immundempende, (Ikke bruk hvis leveraffeksjon, Obs! herpes zoster risiko, Alkoholintoleranse), Tynt lag utenom på slimhinner. Bedring innen 1 uke. Voksne 0,1% x to ganger daglig (barn 0,03%)
- Pimecrolimus (Elidel)
- Imiquimod
- Medikamenter som er under utprøving mot hud-lupus: rituksimab, ruxolitinib, belimumab
- Vitamin-D-mangel (ofte ved lupus) bør korrigeres
CLASI indeks
Graden av hudaffeksjon og alvorlighetsgrad ved hud-lupus kan vurderes ved CLASI- indeks (referanse: Kuhn A, 2010)

